Statins And Cholesterol Controversy: What Evidence Reveals
A Closer Look at the Science and Side Effects

The debate around cholesterol, heart disease, and statin medications continues to evolve as new research emerges.
What was once considered medical dogma – that dietary fat causes heart problems by clogging arteries – has proven far more complex than initially presented to the public.
“People usually don’t understand what dietary fat or cholesterol is,” notes Dr. Malcolm Kendrick, a prominent critic of conventional heart disease models. “They have accepted certain myths that just aren’t true.”
This investigative report examines the controversies surrounding statins, what the latest evidence reveals about their effectiveness and side effects, and explores alternative approaches to cardiovascular health based on emerging science.
What Are Statins & Their Mechanism of Action
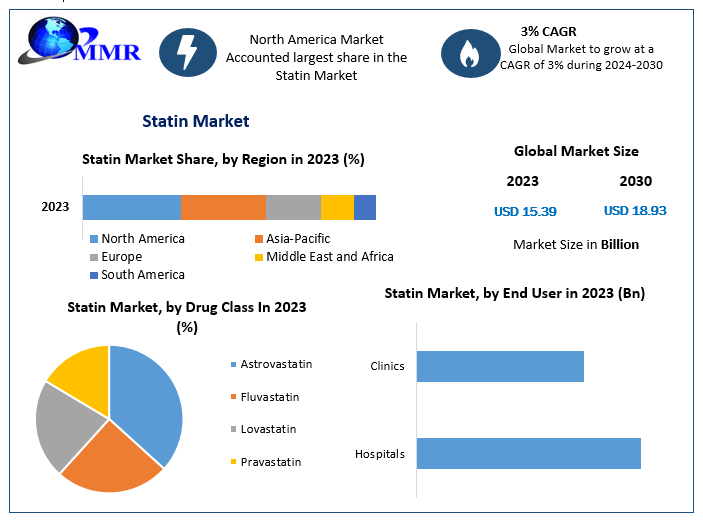
According to Harvard Health Publishing, statins are among the most prescribed medications globally, with over a trillion dollars spent on them to date. But what exactly are these drugs, and how do they work?
Statins function by inhibiting an enzyme called HMG-CoA reductase, which plays a crucial role in cholesterol production. By blocking this enzyme, statins reduce the amount of cholesterol manufactured by the liver, leading to decreased LDL (low-density lipoprotein) levels in the bloodstream.
“They work by blocking a specific enzyme that produces cholesterol called HMG-CoA (hydroxymethylglutaryl-coenzyme A), therefore reducing the amount of cholesterol circulating in your bloodstream,” explains research published in the Journal of Pharmacology & Pharmacotherapeutics.
Commonly prescribed statins include atorvastatin (Lipitor), simvastatin (Zocor), and rosuvastatin (Crestor).
What many patients aren’t told, however, is that the HMG-CoA pathway doesn’t just produce cholesterol – it’s responsible for creating several vital compounds the body needs for optimal function. This single fact helps explain the wide range of side effects observed with these medications.
The Forgotten History of Statins
The discovery of statins dates back to the work of Japanese biochemist Akira Endo in the 1970s, who isolated compounds from fungi that could inhibit cholesterol production. This research eventually led to the development of the first commercial statin, lovastatin, approved by the FDA in 1987. [1]

According to research published in the Proceedings of the Japan Academy, “Statins have revolutionized the treatment of high cholesterol and coronary heart disease. They have been widely prescribed due to their remarkable effectiveness in lowering cholesterol levels and reducing the incidence of heart attacks.”
But were they truly as effective as claimed? And at what cost?
Before statins became the standard treatment for high cholesterol, physicians relied on other approaches. Fibrates, Niacin, and bile acid-binding resins were the primary options, though they had limited effectiveness and their own side effect profiles.
According to the British Heart Foundation, these earlier treatments “modestly lowered LDL cholesterol by 15 to 20%, but there was no evidence that they reduced the risk of heart attack or stroke.”
The question remains: Did statins represent a genuine advancement in cardiovascular medicine, or simply a more profitable approach?
What 900+ Studies Reveal About Statin Safety
Despite their widespread use, an extensive body of research raises serious questions about statin safety. Over 900 studies have documented various adverse effects associated with these medications.
According to these studies, approximately one in five statin users experiences significant side effects. The most commonly reported issues include:
- Muscle damage and pain: Studies from the American College of Cardiology indicate that muscle problems, ranging from mild pain to severe myopathy, affect a substantial percentage of users.
- Cognitive impairment: Perhaps most alarming are the neurological effects. Former NASA astronaut and physician Dr. Duane Graveline experienced this firsthand when he developed global amnesia shortly after starting a statin. “I awoke in the yard of my home with absolute amnesia extending back to my graduate school days,” Dr. Graveline reported. “When I suggested that perhaps my new medicine was the cause of my amnesia, the neurologist replied, almost scoffingly, that ‘Statins do not do that.” After stopping the medication, his symptoms resolved, only to return when he was persuaded to try a lower dose. Research now confirms that cognitive effects can be detected in up to 100% of statin users when sensitive testing methods are employed.
- Increased diabetes risk: Multiple studies have demonstrated that statins significantly increase the risk of developing type 2 diabetes, particularly in women – ironically, the very population often prescribed statins to “protect” against complications. [1][2], [3], [4], [5], [6], [7], [8]
- Liver dysfunction: Before widespread statin use, liver enzyme thresholds for indicating damage were lower. After statins began frequently causing liver problems, these diagnostic thresholds were raised – effectively hiding the problem rather than addressing it. [1], [2]
- Peripheral neuropathy: Research indicates that long-term statin users face a 14 to 26 times higher risk of developing peripheral neuropathy compared to non-users.
But why do these side effects occur? The answer lies in the biochemical pathway statins disrupt.
The Collateral Damage: How Statins Deplete Essential Nutrients
The most significant insight into statin side effects centers on their impact on Coenzyme Q10 (CoQ10). By inhibiting the HMG-CoA reductase pathway, statins not only reduce cholesterol production but also deplete this essential nutrient.
CoQ10 serves two critical functions:
- Powering mitochondria, the energy producers in our cells
- Maintaining cell membrane stability and integrity
“CoQ10 deficiency caused by statins is generally considered the most common cause of their side effects,” notes respected author with pseudonym “A Midwestern Doctor” in his Substack channel, who has extensively documented statin injuries. “This is really sad because those side effects could have been prevented if CoQ10 had been given with the statin.”
Why isn’t CoQ10 supplementation standard practice for statin users? Some critics suggest that recommending supplements would be tantamount to admitting these drugs cause harm – something the pharmaceutical industry has been reluctant to acknowledge.
The energy-related side effects of CoQ10 depletion include chronic fatigue, congestive heart failure, and shortness of breath. Cell membrane integrity issues manifest as muscle breakdown, tendon ruptures, and liver inflammation.
The Cholesterol Hypothesis: Is It Built on Shaky Ground?
For decades, the public has been told that heart disease results from cholesterol “clogging” arteries like grease in a drain pipe. But is this model accurate?
Dr. Malcolm Kendrick, a vocal critic of conventional heart disease theories, argues that the evidence tells a different story. After analyzing risk factors for heart disease, he identified a common thread: most are associated with damage to blood vessel walls and impaired circulation.
Kendrick proposes an alternative model:
- Blood vessels sustain damage from various causes (stress, inflammation, high blood pressure)
- The body repairs this damage using blood clots
- As clots heal, they’re incorporated into vessel walls, with new lining growing over them
- Repeated damage and repair in the same areas leads to abnormal plaques
This model explains several observations that the conventional cholesterol theory struggles with:
- Why plaques form at arterial branch points (areas of greatest stress)
- Why plaques contain the same components found in blood clots
- How cholesterol gets under the arterial lining (it arrives via red blood cells in clots)
“When you examine the components of a plaque, they are found to contain the same debris found in blood clots,” Kendrick notes in his extensive research on the topic.
Perhaps most telling: statins may provide what limited benefit they have not by lowering cholesterol but through their anti-inflammatory properties. They inhibit a key immune system component involved in inflammation called nuclear factor-kappa B (NF-kB).
Could the medical establishment have been focusing on the wrong mechanism all along?
The European Approach: A More Measured Stance
While statins remain widely prescribed in the United States, European medical authorities have adopted a more cautious approach. New European guidelines on statin eligibility have significantly reduced who qualifies for statin therapy.
These guidelines have raised concerns about the dramatic reduction in eligible patients, with some analyses showing that only 4% of the previously targeted population now qualifies for treatment under the new criteria.
While statins are not banned in Europe, the continent’s more measured approach reflects growing skepticism about the universal benefit of these medications and increasing recognition of their risk profiles.
Does this divergence in medical practice suggest that American patients might be overmedicated? The evidence increasingly points in that direction.
How to Optimize Cholesterol Levels Naturally
Given the concerns surrounding statins, many health professionals are advocating for lifestyle-based approaches to cardiovascular health. These strategies focus on addressing the root causes of arterial damage rather than simply lowering cholesterol numbers.
1. Comprehensive Testing
Standard cholesterol tests may not tell the full story. Request advanced lipid profiles that measure particle sizes and inflammatory markers like C-reactive protein.
“It is important to ensure that your doctor conducts a comprehensive lipid profile test, which includes measurements of total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides,” advises cardiologist Dr. Stephen Sinatra, who has long advocated for a more nuanced approach to heart health.
2. Screen for Metabolic Syndrome
Metabolic syndrome – a cluster of conditions including high blood pressure, high blood sugar, excess abdominal fat, and abnormal cholesterol levels – significantly increases cardiovascular risk.
Identifying this condition early allows for targeted interventions that can prevent progression to more serious illness.
3. Focus on Quality Fats


Contrary to decades of low-fat diet advice, research now shows that certain fats are beneficial for heart health.
“Monounsaturated and polyunsaturated fats have been shown to have numerous health benefits,” confirms information from MedlinePlus, the National Library of Medicine’s consumer health resource.
Sources of healthy fats include:
- Avocados
- Olive oil
- Nuts and seeds
- Fatty fish like salmon
4. Manage Blood Sugar
Maintaining stable blood glucose levels is crucial for arterial health. The glycemic load of your diet – how much it raises blood sugar – matters more than just avoiding fat.
Focus on complex carbohydrates, fiber-rich foods, and adequate protein to keep blood sugar steady throughout the day.
5. Prioritize Regular Exercise


Physical activity remains one of the most effective ways to improve cardiovascular health. It increases HDL (beneficial) cholesterol, improves insulin sensitivity, and helps maintain healthy weight.
“Aim for at least 150 minutes of moderate-intensity aerobic activity per week or 75 minutes of vigorous-intensity activity along with strength training exercises at least twice a week,” recommends the American Heart Association.
6. Optimize Sleep Quality
Poor sleep correlates strongly with cardiovascular disease risk. According to the National Heart, Lung, and Blood Institute, inadequate sleep impairs immune function, affects glucose metabolism, and increases inflammation – all factors that can damage blood vessels.
7. Consider Targeted Supplementation
For those concerned about heart health, certain supplements may provide support:
- CoQ10 (especially for statin users)
- Omega-3 fatty acids
- Magnesium (check the best Magnesium supplements)
- Vitamin D (best vitamin D supplements)
- Plant sterols
Always consult with a healthcare provider before starting any supplement regimen.
Frequently Asked Questions
Final Words
The controversy surrounding statins highlights a broader issue in modern medicine: the tendency to rely on pharmaceutical interventions for complex health conditions that may be better addressed through lifestyle modifications and targeted therapies.
The evidence suggests that for many patients – particularly those without established heart disease – the modest benefits of statins may not justify their risks. The one-size-fits-all approach to cholesterol management appears increasingly outdated as our understanding of cardiovascular disease mechanisms evolves.
Those concerned about heart health would be well-served to investigate the endothelial damage model of heart disease and consider comprehensive approaches that address inflammation, metabolic health, and arterial function – not just cholesterol numbers.
As Dr. Kendrick concludes in his research, “Rather than focus on cholesterol, we should focus on the actual causes of endothelial damage and find ways to regain their function.”
Whether statins play a role in your personal health strategy should be a decision made with full awareness of both their potential benefits and their well-documented risks. In an era of personalized medicine, there’s no substitute for an informed partnership between patient and healthcare provider, built on complete and transparent information.
Read Also



