The High-Starch Diet: A Critical Look at the Claims and Potential Dangers
Before you trade fat for carbs, understand the significant risks to your metabolic health and waistline
Remember the low-fat craze of the 1990s? America got fatter. Now a new wave of dietary advice pushes extreme carbohydrate consumption through high-starch diets, claiming miraculous weight loss and disease reversal.
The pitch sounds familiar: eat unlimited amounts of potatoes, rice, and pasta while strictly limiting fats and proteins.
But mounting evidence suggests this approach might create more metabolic problems than it solves.
What Is a High-Starch Diet? A Look Beneath the Surface
At its core, a high-starch diet makes starches = the foundation of your eating pattern. We’re talking about 70-90% of calories from potatoes, rice, corn, and similar foods, with minimal fat (often under 10%) and restricted protein.
The diet is 90% starch-based. It is based on a variety of starches such as rice, potatoes, corn, breads, pasta1.
Proponents emphasize “whole” starches over refined ones. The argument goes that brown rice and sweet potatoes differ fundamentally from white bread. But here’s what they don’t tell you.
Even whole starches deliver a massive glucose load to your system. All starches, even “healthy” grains, create after-meal glucose and insulin spikes2.
Even seemingly healthy food choices (whole grain bread, brown rice, and whole wheat pasta, for example) can lead to increases in blood sugar and insulin2.
A large baked potato can spike blood sugar as much as pure glucose in some individuals.
Anti-nutrients present another hidden problem. Grains and legumes contain compounds like lectins and phytates that interfere with mineral absorption. Your “healthy” whole grains might actually block your body from absorbing essential nutrients like iron, zinc, and calcium.
Deconstructing the Claims: Is There Fire Behind the Smoke?
Claim 1: “Effortless Weight Loss”
The initial weight loss on high-starch diets comes from extreme calorie restriction and water loss, not metabolic magic. When you eliminate all oils, limit protein, and eat monotonous meals of plain starches, you naturally eat less. Any diet this restrictive causes weight loss initially.
But what happens long-term? The extreme nature makes compliance nearly impossible. (Ed. note: This sustainability issue affects most participants according to multiple sources.)
As with any restrictive low-fat diet, it may lead to flatulence, possibly poor mineral absorption from excess fiber, and limited food choices that may lead to a feeling of deprivation1.
Once people resume normal eating patterns, the weight returns – often with interest.
Claim 2: “Reverses Chronic Disease”
He was even claiming that a high-starch diet could be used to treat chronic diseases such as arthritis, cancer, diabetes, osteoporosis, and heart disease3. Yet where’s the robust scientific evidence? Many claims were made without supporting evidence3.
The improvements some people experience likely come from eliminating processed foods and refined oils, not from eating massive amounts of starch. When you stop eating junk food, you feel better—shocking, right?
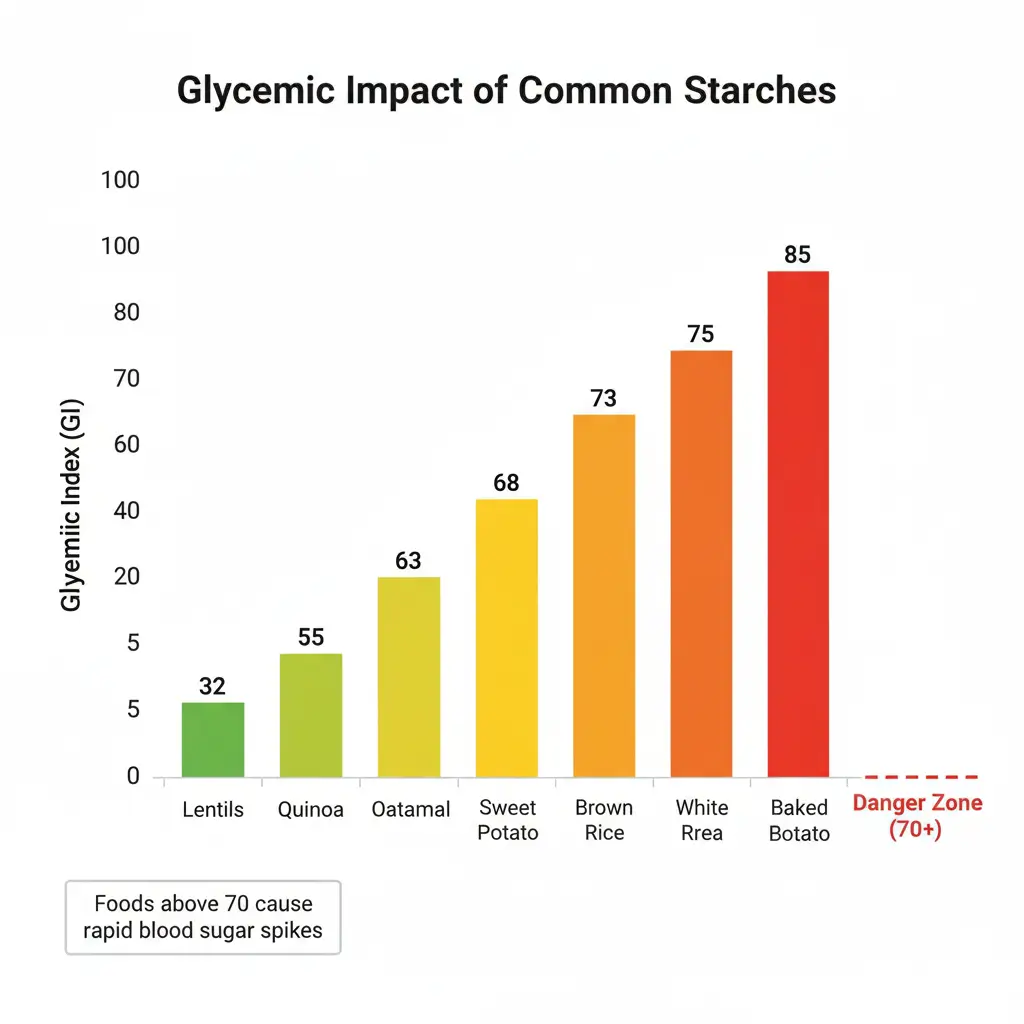
Check Your Starch’s Impact
The Blood Sugar Rollercoaster: The Biggest Risk
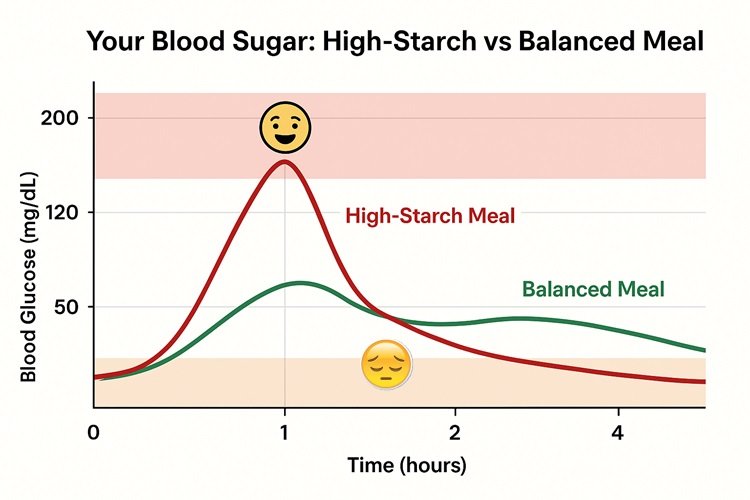
"Won't all those carbs spike my blood sugar?" Absolutely.
Rapidly digestible starch elevates postprandial glycemia and impinges glycemic homeostasis, elevating the risk of developing T2D4. Many adults today suffer from some degree of carbohydrate intolerance = they don't handle large amounts of carbs well. This becomes especially problematic for those who are overweight or sedentary.
Here's what happens when you flood your system with starch:
- Massive insulin spike: Your pancreas pumps out insulin to deal with the glucose flood
- Blood sugar crash: What goes up must come down, leaving you tired and hungry
- Chronic hyperinsulinemia: Repeatedly high insulin levels drive fat storage and inflammation
The fasting serum insulin levels were higher in the OVX than the sham rats, and in the OVX rats, a high SU diet increased the serum insulin levels more than a high ST diet5. This chronic elevation of insulin represents a key driver of insulin resistance and Type 2 diabetes.
The danger compounds over time. T2D is defined as chronic elevations in blood glucose concentrations due to insulin resistance or impaired insulin secretion4.
By constantly challenging your body with massive starch loads, you're essentially training it to become insulin resistant.
A Case Study in Dogma: The McDougall Program
The most prominent example of extreme starch advocacy comes from Dr. John McDougall's "Starch Solution." His book The McDougall Plan was on New York Times paperback "Advice, How-to, and Miscellaneous" bestseller list.
The plan is classified as a low-fat fad diet in Wardlaw's Perspectives in Nutrition. McDougall has been criticized for making unsubstantiated health claims1.
The program demands rigid adherence: no oils, vegan-only, starch-centered meals. The diet rejects all animal products as well as cooking oils, processed food, alcoholic beverages and caffeinated drinks1.
This all-or-nothing approach raises red flags.
Doctor Harriet Hall wrote that the book is filled with anecdotes and questionable statements, and that it makes many claims which are not supported by science. Hall concluded that "Some of McDougall's recommendations are in line with mainstream advice, but there is reason to fear that strict adherence to his whole Program might result in nutritional deficits that could do more harm than good"3.
Its severe restrictions make it nutritionally questionable and it has never been properly tested in a controlled study3.
"But what about all the success stories?" Anecdotes aren't evidence. Without controlled trials comparing the diet to other approaches, we can't determine whether benefits come from the starch itself or simply from eliminating processed foods.
The Unspoken Dangers: What Proponents Don't Tell You
Let's examine the nutritional gaps this diet creates:
- Critical nutrient deficiencies: While plant-based diets are rich in nutrients such as fiber, vitamin C, folate, and magnesium, nutrient deficiencies including that of vitamin D, iron, omega-3 polyunsaturated fatty acids, and vitamin B12 can occur6. Vitamin B12 deficiencies are common in individuals consuming plant-predominant diets, including those who consume dairy and/or eggs6.
- B12 crisis: Vitamin B12 is unique in that it is only synthesized by microorganisms and thus essentially devoid in foods of plant origin6. Without supplementation, deficiency becomes inevitable, leading to anemia and potentially irreversible nerve damage.
- Omega-3 shortage: Plant sources don't provide EPA and DHA = the forms your brain actually needs. The conversion from plant-based ALA remains extremely inefficient.
- Fat-soluble vitamin problems: Without dietary fat, your body struggles to absorb vitamins A, D, E, and K. These vitamins play crucial roles in immunity, bone health, and cellular function.
- Potential muscle loss: Combining very low fat with potentially inadequate protein creates a perfect storm for sarcopenia. Less muscle means slower metabolism and increased frailty as you age.
- The sustainability disaster: Nutritionist Fredrick J. Stare and epidemiologist Elizabeth Whelan criticized its restrictive regime and "poor advice", concluding that the diet's concepts were "extreme and out of keeping with nutritional reality". The authors state that failure to consume dairy products creates a risk for osteoporosis, and that if animal products cannot be replaced with peanut butter and soybean foods, vegans may not obtain enough protein1.
Critical Nutrient Deficiencies Alert
Zero B12 in plant foods. Your body needs 2.4 mcg daily for nerve function and DNA synthesis.
⚠️ Consequences: Irreversible nerve damage, anemia, cognitive decline
Plant sources provide ALA only. Your brain needs EPA/DHA - conversion rate less than 5%.
⚠️ Consequences: Depression, cognitive decline, inflammation
Without dietary fat (under 10% on this diet), absorption of these vitamins drops by 80%.
⚠️ Consequences: Weakened immunity, bone loss, poor wound healing
Phytates in grains block mineral absorption. Plant iron (non-heme) absorbs at only 2-20% efficiency.
⚠️ Consequences: Fatigue, weakened immunity, hair loss
What About the Blue Zones? Debunking the High-Starch Myth
"Don't the longest-lived populations eat high-starch diets?" Not exactly.
Blue Zone populations like Okinawans and Sardinians do include starches in their diets. But attributing their longevity to starch alone ignores crucial context:
- Constant physical activity throughout the day
- Strong social connections and low stress
- Complete absence of processed foods
- Genetic adaptations developed over millennia
- Moderate portion sizes
Their traditional diets also included fish, small amounts of meat, and fermented foods - hardly the vegan starch-fest being promoted. Modern Okinawans eating more Western-style foods have seen their legendary health advantages disappear.
Context matters. Your sedentary office job and Netflix habits don't match the lifestyle of traditional farming communities.
High-Starch vs Balanced: The Real Comparison
| Factor | High-Starch Diet | Balanced Approach |
|---|---|---|
| Blood Sugar | ⚠️ Severe spikes & crashes. Insulin levels 2-3x higher after meals | ✓ Stable levels. Minimal insulin response |
| Nutrient Status | ⚠️ Missing B12, Omega-3, low mineral absorption | ✓ Complete nutrition from varied sources |
| Satiety | ⚠️ Hungry 2-3 hours after eating | ✓ Satisfied 4-6 hours between meals |
| Energy Levels | ⚠️ Energy crashes, afternoon fatigue | ✓ Steady energy throughout the day |
| Long-term Risk | ⚠️ Increased diabetes risk, metabolic syndrome | ✓ Improved metabolic health markers |
| Sustainability | ⚠️ Extremely restrictive, social isolation | ✓ Flexible, socially compatible |
A Smarter, Safer Approach to Carbohydrates
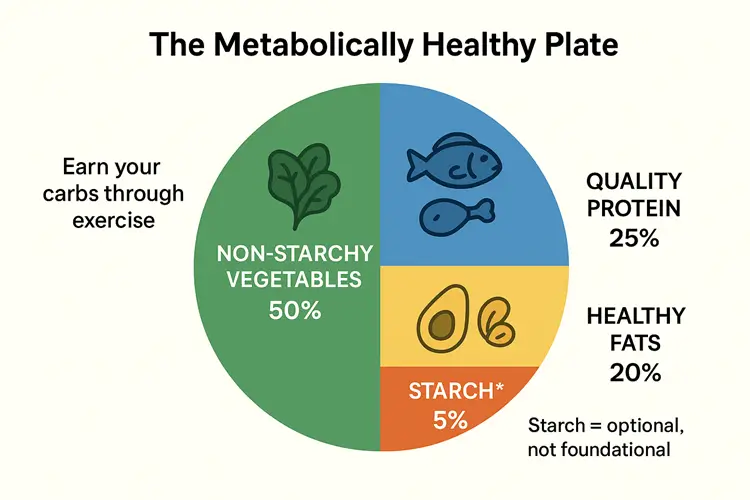
Instead of making starch the foundation of your diet, consider a more balanced approach:
- Prioritize nutrient density: Build meals around non-starchy vegetables, quality proteins, and healthy fats. These foods provide essential nutrients without the blood sugar rollercoaster.
- Use starch strategically: Earn your carbs through physical activity. A small portion of sweet potato after a workout differs vastly from eating pounds of potatoes while sedentary.
- Focus on low-glycemic choices: If you include starches, opt for smaller portions of foods with lower glycemic impact. Legumes and steel-cut oats beat white rice and instant mashed potatoes.
- Monitor your response: Check your blood sugar response to different foods. What works for one person might send another's glucose soaring.
FAQ: Answering Your Lingering Doubts
A Risky Bet Not Worth Taking
The high-starch diet represents an extreme swing of the dietary pendulum. While born from good intentions—eating more whole foods—its rigid nature and disregard for individual carbohydrate tolerance make it potentially harmful for most people.
The evidence shows clear risks: blood sugar dysregulation leading to insulin resistance, critical nutrient deficiencies requiring lifelong supplementation, and sustainability challenges that doom long-term success. The concepts in this book are extreme and out of keeping with nutrition reality. The diet is nutritionally precarious and, we hope, too austere for anyone to think about trying to follow3.
Rather than gambling your metabolic health on an extreme approach that eliminates entire food groups, adopt a truly balanced strategy. Manage your carbohydrate intake based on your activity level and metabolic health. Include adequate protein and healthy fats. Focus on nutrient density over ideology.
Your body deserves better than riding the blood sugar rollercoaster. Choose metabolic stability over dietary extremism. The boring middle ground of balanced nutrition might not sell books, but it builds lasting health.
References
- [1] PMC - "Resistant starch and type 2 diabetes mellitus: Clinical perspective" - April 2024
- [2] PMC - "A comparison of the effects of resistant starch types on glycemic response" - April 2023
- [3] Life Extension - "How To Prevent Sugar Spikes Caused By Starch Diets" - October 2024
- [4] PMC - "Resistant starch can improve insulin sensitivity independently of the gut microbiota" - February 2017
- [5] PMC - "Effects of the resistant starch on glucose, insulin, insulin resistance, and lipid parameters" - June 2019
- [6] News Medical - "Resistant starch diet proves a game changer for weight loss and diabetes control" - February 2024
- [7] PubMed - "Effects of resistant starch on glycemic response, postprandial lipemia and appetite" - April 2023
- [8] ScienceDirect - "Hypoglycemic effect of recrystallized resistant starch" - February 2024
- [9] PMC - "A High Carbohydrate Diet Induces Insulin Resistance" - August 2015
- [10] PMC - "Role of resistant starch on diabetes risk factors in people with prediabetes" - March 2018
- [11] Goodreads - "The Starch Solution by John McDougall" - 2024
- [12] Weston A. Price Foundation - "The Starch Solution Review" - November 2019
- [13] Wikipedia - "John A. McDougall" - Updated 2024
- [14] Science-Based Medicine - "The McDougall Diet" - October 2020
- [15] Lani Muelrath - "My McDougall Diet Failure" - June 2015
- [22] Healthline - "Vitamin B12 Foods: 12 Great Sources" - February 2024
- [23] PMC - "Vitamin B12 and Plant-Predominant Diets" - June 2022
