High Cholesterol and Heart Disease: Myth or Truth? Why the Science Has Changed
Are we treating the fire or the firefighter? We analyze 50 years of buried data to reveal why lowering cholesterol might not save your life - and what actually will.
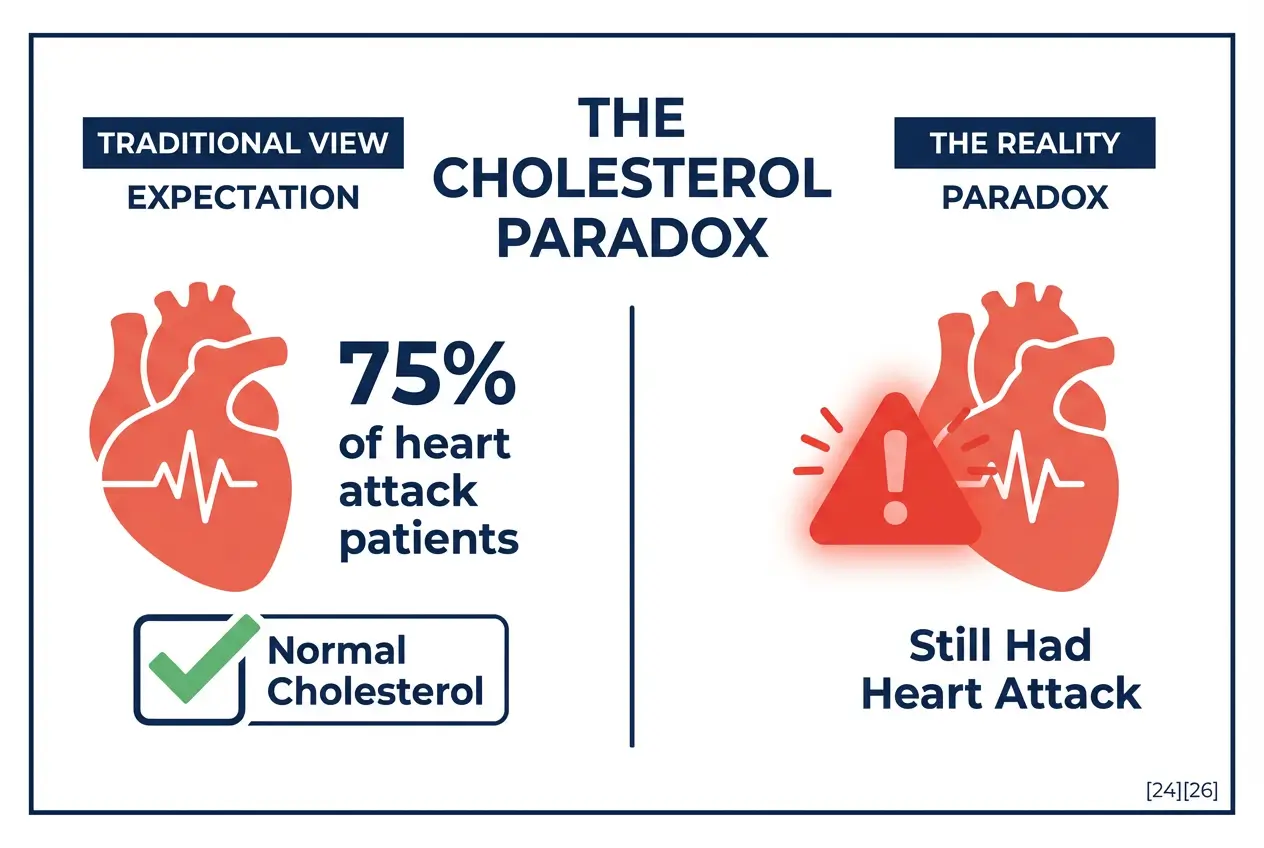
If cholesterol causes heart attacks, why do 75 percent of heart attack patients have “normal” cholesterol levels? [24][26]
About half of all heart attack victims walk into the emergency room with LDL levels under 100 mg/dL. [24][30]
That’s classified as “optimal” by current guidelines. Another shocking fact: 50 percent of people with ideal cholesterol have dangerous plaque buildup in their arteries.[28]
Something doesn’t add up.
For 50 years, doctors prescribed the same advice.
- Lower your cholesterol.
- Eat less fat.
- Take statins.
The message was simple. Cholesterol clogs your arteries like grease in a pipe. High cholesterol kills you. Low cholesterol saves you.
But the data tells a different story. A story that drug companies and health authorities buried for decades. A story that costs patients billions while their muscle pain, brain fog, and diabetes risk climb every year.
You were told cholesterol is the gun. The evidence shows it might be the ambulance arriving at the crime scene.
The Origin of the Fraud
Ancel Keys changed American medicine with one study.
The Seven Countries Study in 1970 claimed to prove that saturated fat raises cholesterol and causes heart disease. Countries that ate more fat had more heart attacks. Simple correlation equals causation. Problem solved.

Except Keys ignored 16 other countries. [1]
He cherry-picked data that fit his hypothesis.
France ate saturated fat but had low heart disease rates. Switzerland consumed butter and cheese but lived longer than Americans. Keys excluded them. He published only the countries that made his theory work.
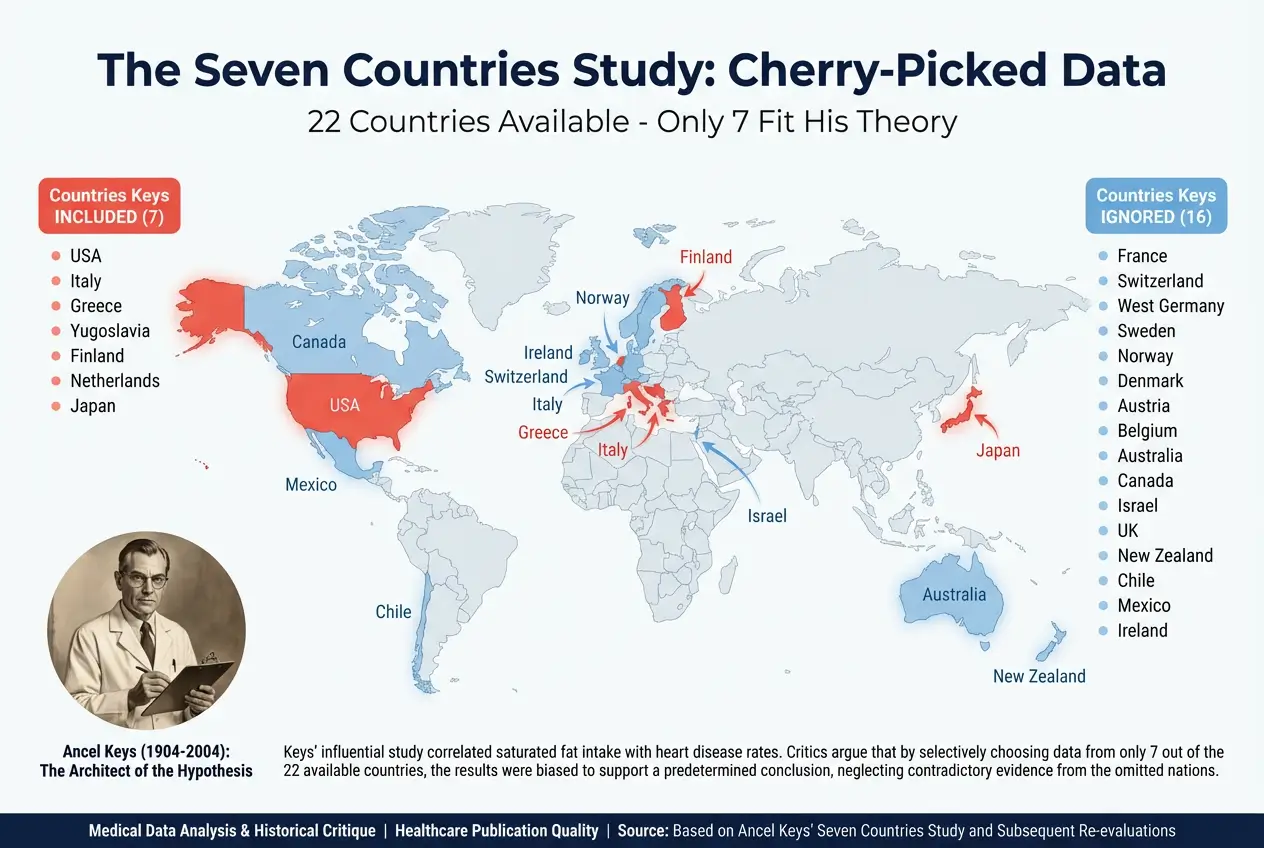
Other scientists challenged him. British researcher John Yudkin blamed sugar, not fat, for heart disease. [8] The data supported Yudkin. But Keys had influence, funding, and political connections. His theory won. Sugar got a pass. Fat became the enemy.
The Diet-Heart Hypothesis became gospel. Federal guidelines recommended vegetable oils over butter. Margarine replaced real food. Processed seed oils flooded the market. Americans cut saturated fat by 20 percent between 1970 and 2000.
Heart disease rates barely changed.
The Smoking Gun They Buried
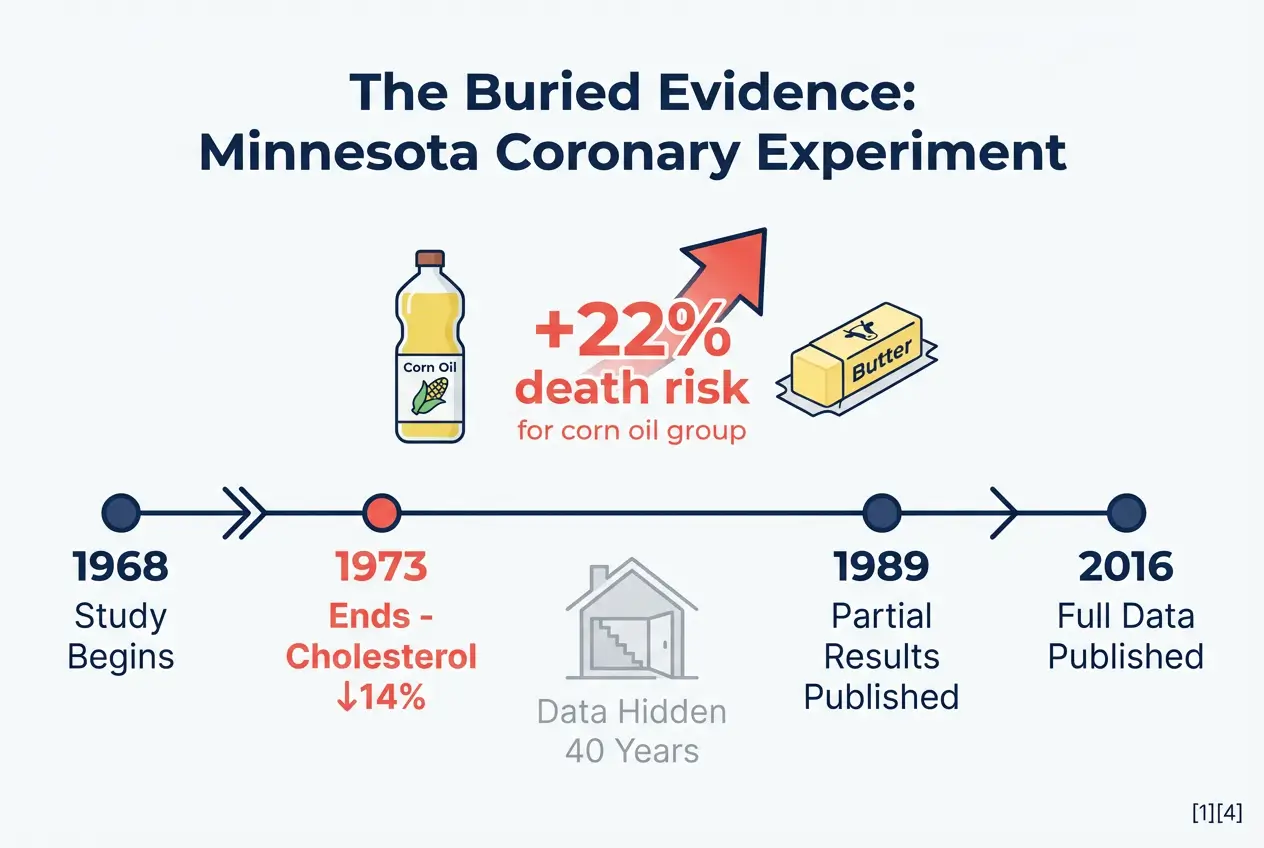
The Minnesota Coronary Experiment should have ended the debate in 1973. [1][4][5]
Researchers ran a controlled trial at six mental hospitals and one nursing home in Minnesota. They fed 9,423 patients either saturated fat or corn oil. The corn oil group ate vegetable oil instead of butter. The experiment lasted 4.5 years.[10]
The hypothesis was clear. Replacing saturated fat with vegetable oil would lower cholesterol. Lower cholesterol would reduce heart attacks and deaths. Everyone would live longer.
Cholesterol dropped 14 percent in the corn oil group. [4]
That part worked. Blood tests confirmed it. The Diet-Heart Hypothesis predicted victory.
But people in the corn oil group didn’t live longer. They died faster. [3][4]
For every 30-point drop in cholesterol, death risk jumped 22 percent. [4]
Among elderly patients over 65, the corn oil diet killed more people within two years. [3]
Autopsies showed no reduction in atherosclerosis. Heart attacks occurred at the same rate. [1][5]
The lead researcher, Dr. Ivan Frantz Jr., never published the complete results. He sat on the data for 16 years. When asked why, he told a journalist he was “disappointed” the study didn’t support his theory. [6]
The data sat in a basement for 40 years. In 2016, NIH researcher Christopher Ramsden found the original computer tapes in the son’s mother’s basement. [4][8]
He published the analysis in the British Medical Journal.
The vegetable oil lowered cholesterol but didn’t save lives. [1][5]
The evidence contradicted five decades of nutritional advice.
Nobody apologized.
The Statistical Trick That Sells Drugs
Drug companies use one deceptive tactic to sell statins. They report “Relative Risk” instead of “Absolute Risk“. [11][14]
Relative Risk sounds impressive. “This drug reduces heart attacks by 36 percent!” Headlines love this number. Doctors repeat it. Patients hear 36 percent and think one-third of people avoid heart attacks.
Wrong.
Absolute Risk tells the truth. In clinical trials, heart attack rates drop from 3 percent to 2 percent. [6][8][10]
That’s a 1 percent actual benefit. The Relative Risk calculation takes the difference (1 percent) and divides it by the original rate (3 percent). The result is 33 percent. Marketers round up to 36 percent.
Both numbers describe the same outcome. One sounds life-saving. The other sounds like rounding error.
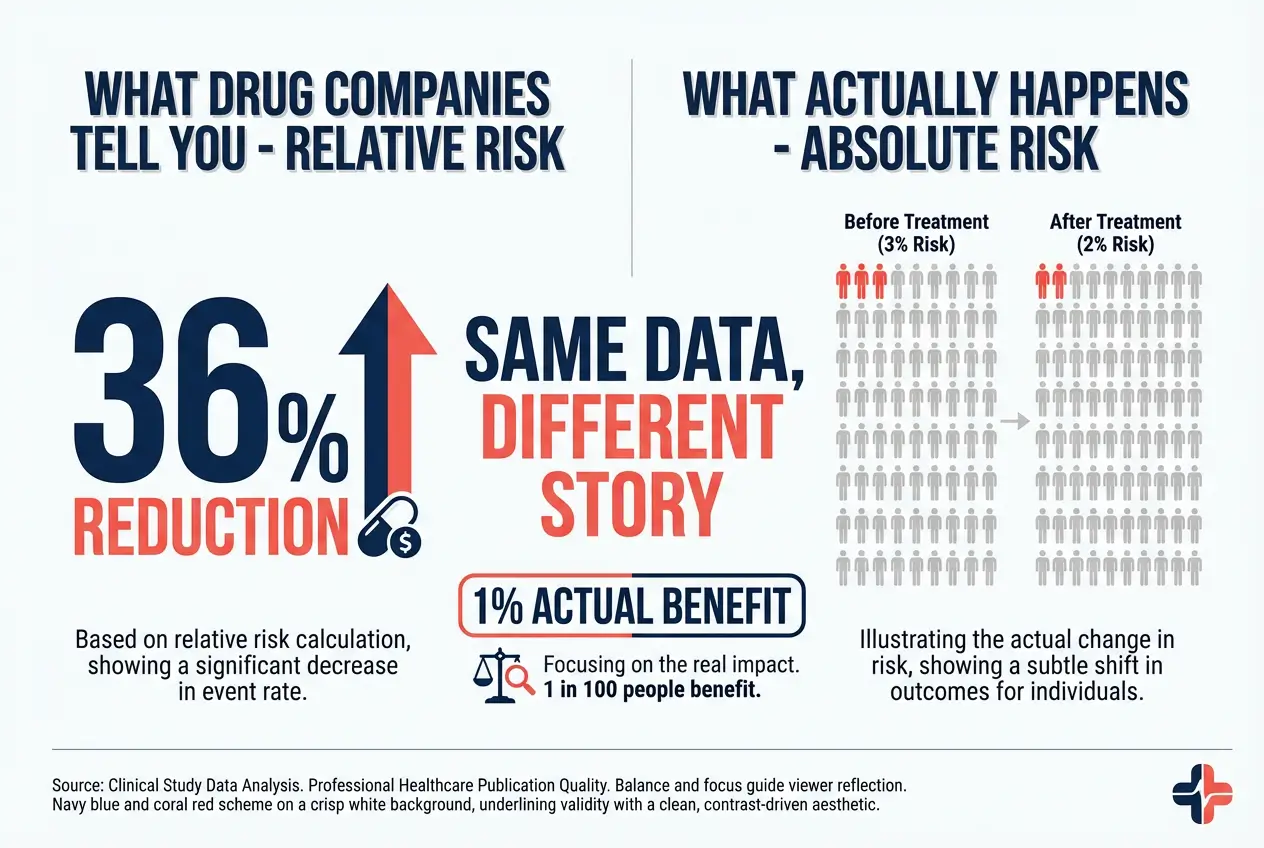
Number Needed to Treat (NNT) exposes the scam. [11][12][14]
The NNT tells you how many people must take the drug for one person to benefit. For statins in low-risk patients, the NNT ranges from 60 to 217 for preventing one non-fatal heart attack over five years. [11][12]
That means 60 to 217 people swallow pills daily for five years. One person avoids a heart attack. The other 59 to 216 people get zero benefit. They paid money. They risked side effects. They got nothing in return.
For all-cause mortality in low-risk groups, statins show no benefit. [11] You don’t live longer. You just take expensive pills.
The NNT for preventing death is even worse. Some studies show 167 patients need treatment for 4.1 years to prevent one death. [14]
At that rate, the 166 other patients might develop diabetes, muscle damage, or cognitive decline before they see any benefit.
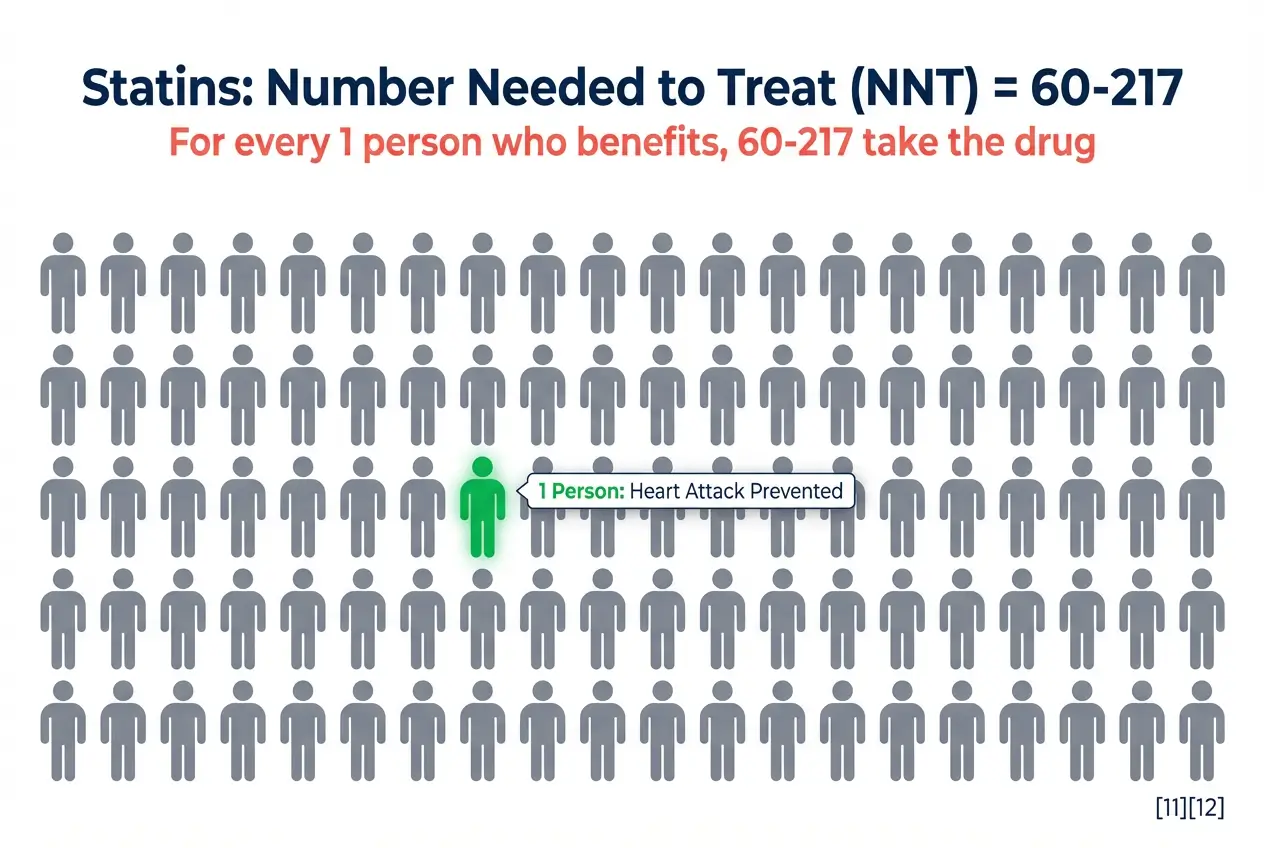
Studies show statins increase diabetes risk by 9 percent. The Number Needed to Harm for diabetes is 204 over five years. The Number Needed to Harm for muscle damage is 21. [11]
You have a one in 21 chance of muscle pain. You have a one in 204 chance of diabetes. You have a one in 60 to 217 chance of avoiding a non-fatal heart attack.
The math doesn’t favor you.
Cholesterol Doesn’t Clog Pipes
Your arteries are not copper plumbing. They’re living tissue with complex immune responses.
The “cholesterol clogs arteries” analogy fails basic biology. Plaque doesn’t build up like grease in a drain. Atherosclerosis is an inflammatory repair process. [4]
The Response to Injury theory explains the mechanism. Something damages the arterial wall. Smoking, sugar, oxidized LDL, or chronic stress injures the endothelium (the inner lining of blood vessels). Your body detects the damage and sends repair materials. [4]
Cholesterol arrives as part of the repair crew. It patches the damaged area like a scab on a cut. Clotting factors stabilize the injury. The body tries to heal itself.
Blaming cholesterol for plaque is like blaming firefighters for the fire. Yes, they’re at the scene. No, they didn’t cause the damage.
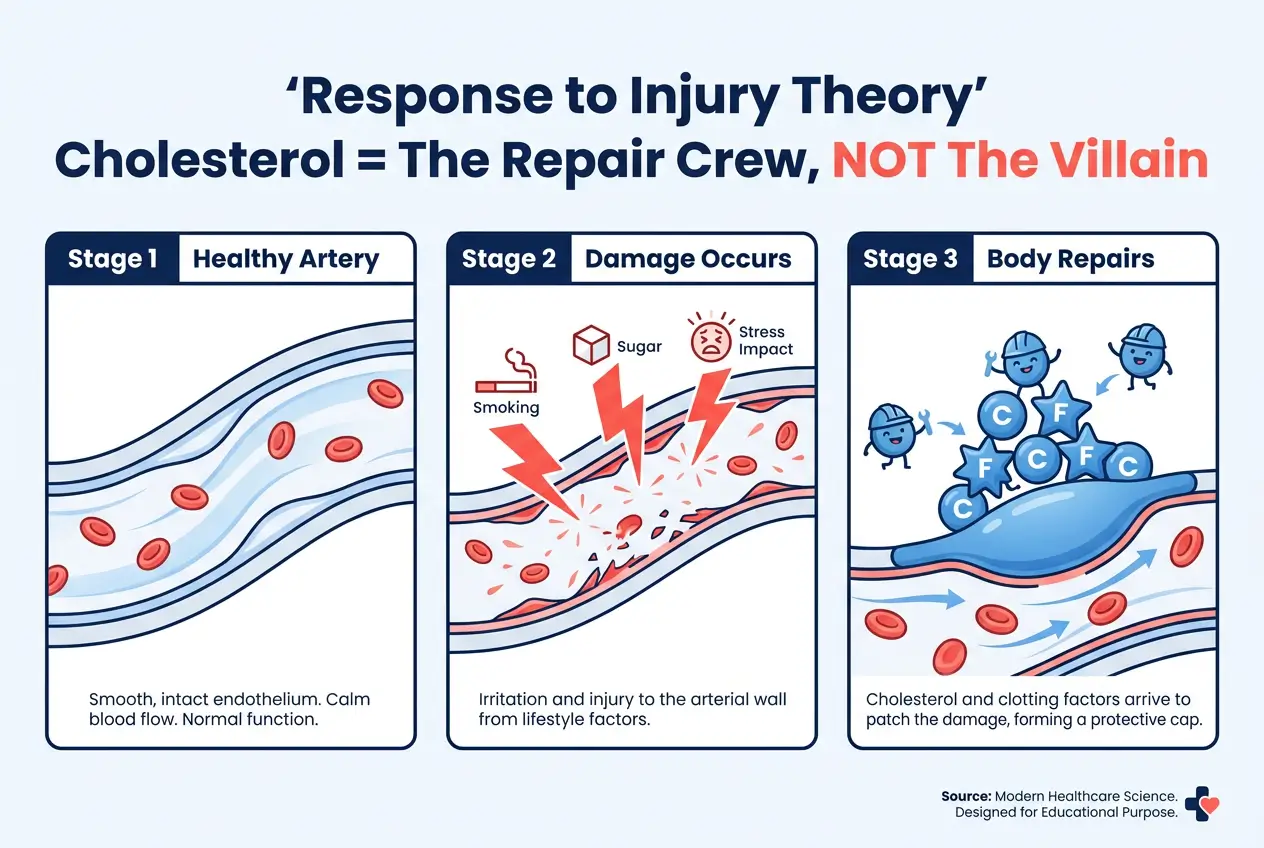
If cholesterol were the villain, everyone with high cholesterol would develop heart disease. They don’t. Plenty of people with total cholesterol over 250 mg/dL live into their 90s without cardiovascular events. Meanwhile, people with cholesterol under 160 mg/dL die of heart attacks. [24][25][26]
The correlation breaks down when you examine individual cases. Something else drives the disease.
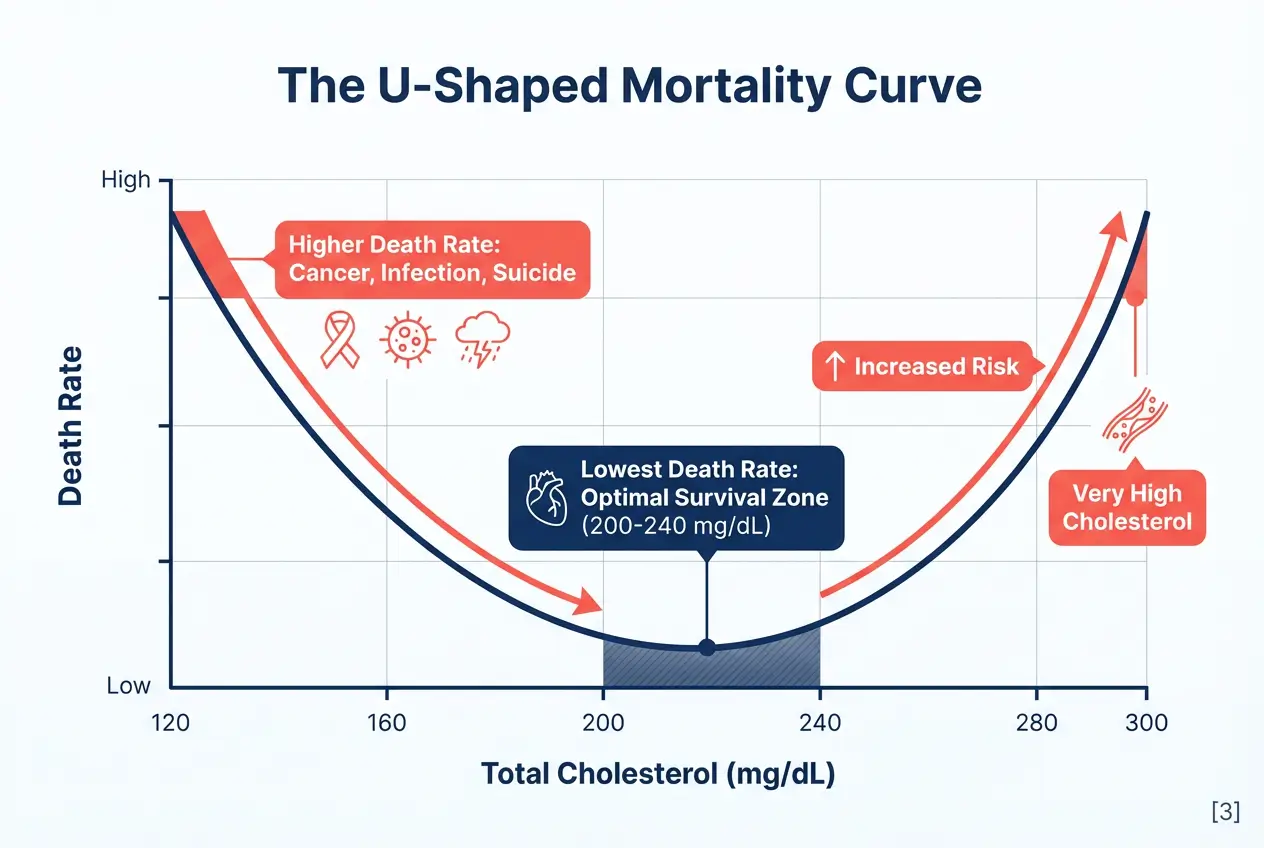
The U-Shaped Mortality Curve
Lower cholesterol is not always healthier. Multiple studies show a U-shaped curve for mortality. [3]
People with very low cholesterol (under 160 mg/dL) die at higher rates than people with moderate cholesterol (200–240 mg/dL). [3] The lowest death rates occur in the middle range. Both extremes increase risk.
Why would low cholesterol kill you? Cholesterol serves critical functions.
Your brain is 25 percent cholesterol. Every cell membrane requires it. Sex hormones are made from cholesterol. Vitamin D synthesis depends on cholesterol. Your immune system uses cholesterol to bind and neutralize bacterial toxins. [2]
Low cholesterol correlates with higher rates of cancer, infection, and suicide. [2]
Aggressive statin use in elderly patients increases cognitive decline and dementia risk. [1][2][36]
Some patients develop transient global amnesia, a sudden memory loss that resolves after stopping the drug. [36]
Your body doesn’t make cholesterol to hurt you. It makes cholesterol because you need it to survive.
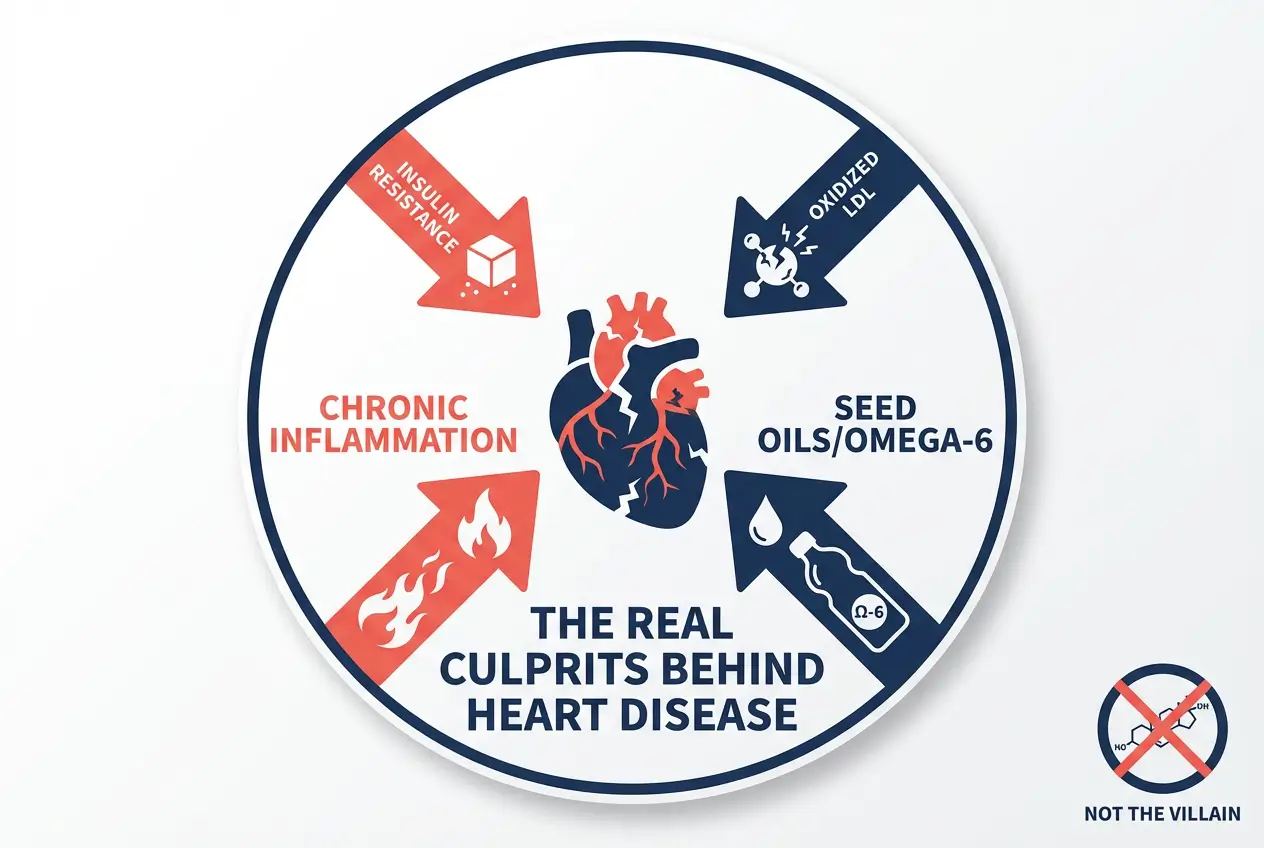
The Real Culprits
If cholesterol isn’t the gun, what’s pulling the trigger?
Insulin Resistance
High blood sugar damages arteries through glycation. [4] Glucose molecules attach to proteins in the arterial wall. The proteins become stiff and dysfunctional. This process accelerates plaque formation.
Insulin resistance precedes most heart attacks. Your Triglyceride-to-HDL Ratio predicts heart disease better than total cholesterol. [24][30] A ratio above 2:1 signals metabolic dysfunction. Below 1:1 is ideal.
Oxidized LDL
Not all LDL is dangerous. Large, fluffy LDL particles float harmlessly through your bloodstream. Small, dense LDL particles penetrate the arterial wall and oxidize. Oxidized LDL triggers inflammation and immune responses. [4]
Standard cholesterol panels don’t measure particle size. They report total LDL. A person with 120 mg/dL of large LDL has lower risk than someone with 100 mg/dL of small, dense LDL.
Testing for ApoB (a protein marker for particle number) gives better risk assessment than LDL alone.
Chronic Inflammation
Elevated high-sensitivity C-reactive protein (hs-CRP) indicates systemic inflammation. Stress, poor sleep, chronic infections, and processed foods drive inflammation higher. Inflammation damages the endothelium and starts the atherosclerotic cascade.
Seed Oils
Vegetable oils high in omega-6 fatty acids (corn oil, soybean oil, canola oil) promote inflammation when consumed in excess. [1][2] The omega-6 to omega-3 ratio in the American diet shifted from 1:1 to 20:1 over the past century. This imbalance fuels chronic disease.
The Minnesota Coronary Experiment proved this. Corn oil lowered cholesterol but increased deaths. [1][3][4] The mechanism likely involves oxidized omega-6 fatty acids damaging arterial walls.
What Statins Actually Do
Statins block the Mevalonate Pathway. This pathway produces cholesterol. Blocking it lowers LDL. That’s the intended effect.
But the Mevalonate Pathway also produces CoQ10, an enzyme critical for energy production in every cell. [31][33][35][38]
CoQ10 Depletion
Your heart needs CoQ10 to generate ATP (cellular energy). Muscles need it to contract. Brain cells need it to function. Statins reduce CoQ10 levels by 30–40 percent in blood and muscle tissue. [31][33][35][38]
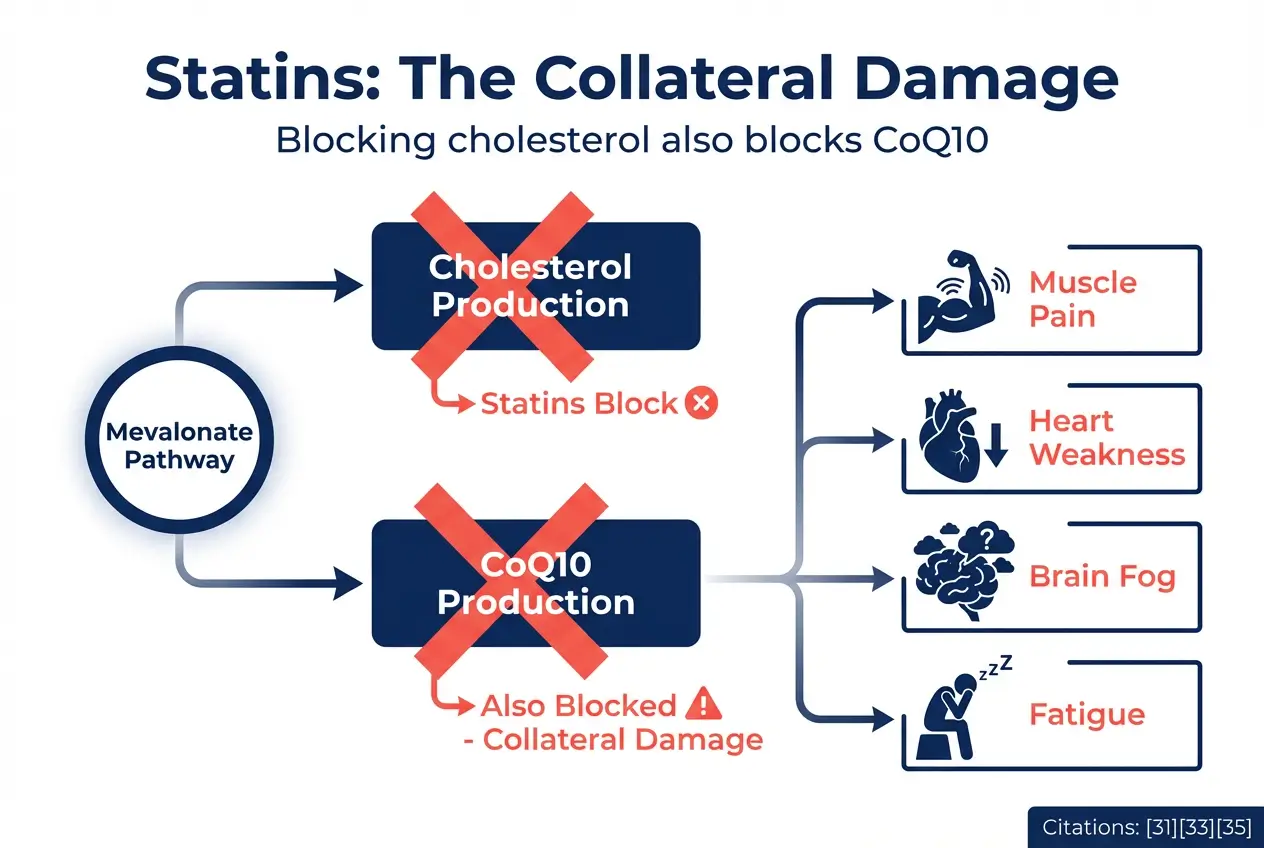
Muscle pain affects 5–10 percent of statin users in clinical trials. [32] Real-world surveys show 30–60 percent experience muscle symptoms. [35] The discrepancy exists because trials don’t ask about symptoms proactively. [11] Patients report pain, weakness, cramping, and fatigue. [37]
CoQ10 depletion explains the mechanism. Muscle cells can’t produce enough ATP. They fatigue faster. Some patients develop rhabdomyolysis, a life-threatening muscle breakdown. [31][33]
Meta-analyses show CoQ10 supplements reduce muscle pain in statin users. [37] The effect is modest but real.
Diabetes Risk
Statins increase insulin resistance. [11] They raise blood sugar. They push borderline diabetics into full diabetes. The absolute risk increase is 0.49 percent over five years, or a Number Needed to Harm of 204. [11]
This creates a perverse cycle. You take statins to prevent heart disease. The statins give you diabetes. Diabetes increases heart disease risk. Now you need more medication.
Cognitive Decline
Case reports describe statin-induced memory loss, confusion, and brain fog. [2][36] The FDA added cognitive impairment warnings to statin labels in 2012. Some patients experience reversible cognitive decline that resolves after stopping the drug. [36]
Your brain is 25 percent cholesterol. Neurons require cholesterol for synapse formation and neurotransmitter function. Aggressive cholesterol lowering may impair brain health, especially in elderly patients. [2]
The Numbers That Actually Matter
Stop obsessing over total cholesterol. These markers predict risk better.
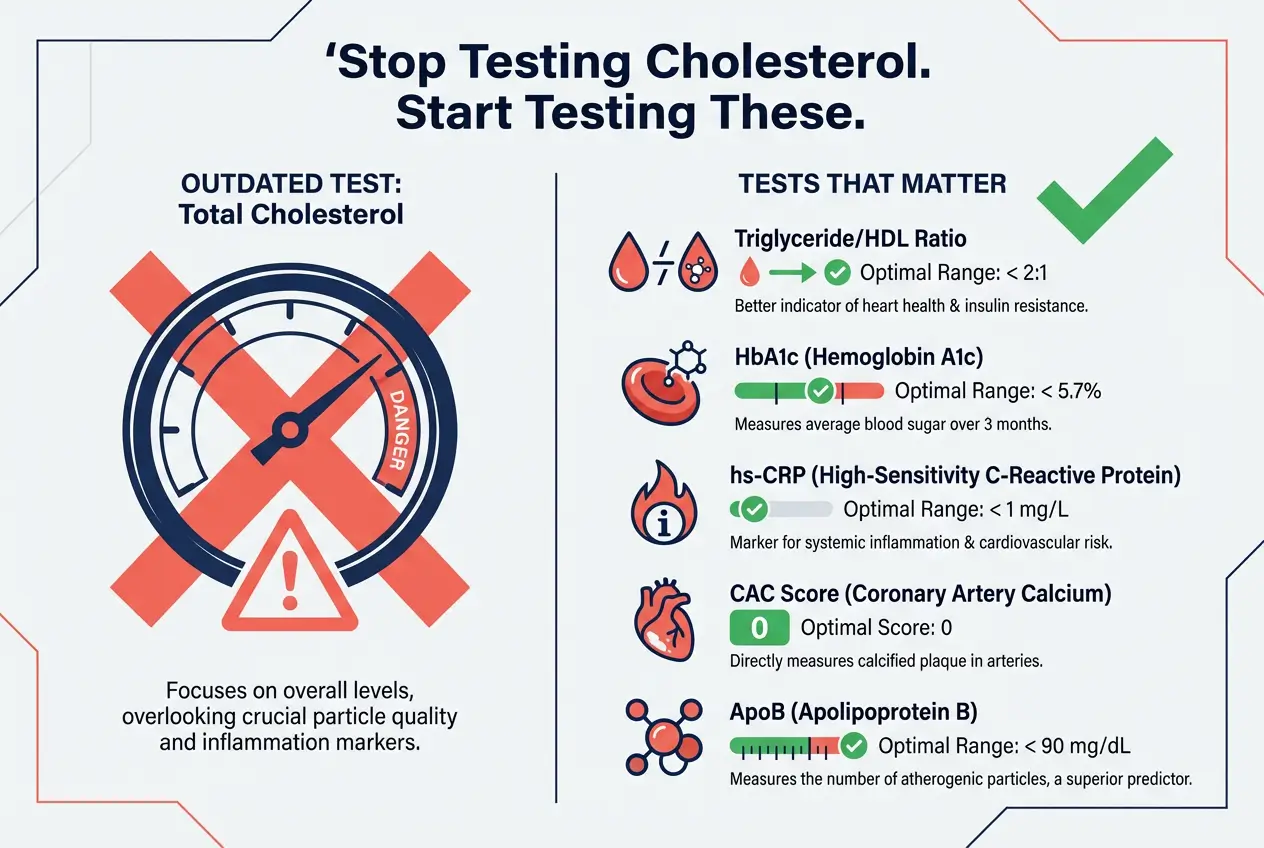
- Triglyceride-to-HDL Ratio: Divide your triglycerides by your HDL. A ratio under 2:1 is healthy. Under 1:1 is ideal. Above 3:1 signals insulin resistance and increased heart disease risk. [24][30] This ratio outperforms total cholesterol for predicting cardiovascular events.
- HbA1c: Your three-month average blood sugar. Anything above 5.7 percent indicates prediabetes. Above 6.5 percent is diabetes. Elevated HbA1c damages arteries through glycation, regardless of cholesterol levels.
- High-Sensitivity C-Reactive Protein (hs-CRP): Measures systemic inflammation. Levels above 3 mg/L indicate high cardiovascular risk. Below 1 mg/L is ideal.
- Coronary Artery Calcium (CAC) Score: The only test that shows actual disease, not just risk factors. A CT scan measures calcium deposits in your coronary arteries. A score of zero means no detectable plaque. Higher scores indicate more disease. CAC score predicts heart attacks better than any blood test. It separates people with real atherosclerosis from people with elevated cholesterol who will never develop disease.
- ApoB: Measures the number of atherogenic particles in your blood. ApoB counts LDL, VLDL, and remnant cholesterol particles. It predicts risk better than LDL alone. Remnant cholesterol (calculated as total cholesterol minus LDL minus HDL) predicts heart attack risk independent of LDL. Levels above 24 mg/dL increase risk by 40–50 percent.[29]
What Actually Works
Real food. Movement. Sunlight. Sleep. Stress management.
Processed sugar damages your arteries more than saturated fat. Eliminate refined carbohydrates. Eat meat, fish, eggs, vegetables, and whole foods your great-grandmother would recognize.
Saturated fat from natural sources (butter, beef, coconut oil) is not your enemy. Your body uses it for hormone production, cell membranes, and energy. The Minnesota Coronary Experiment proved vegetable oils are more dangerous than animal fats. [1][3][4]
Sunlight produces nitric oxide, which dilates blood vessels and lowers blood pressure naturally. Get 20 minutes of sun exposure daily without sunscreen. Your vitamin D levels will thank you.
Exercise improves insulin sensitivity, reduces inflammation, and strengthens your heart. Resistance training builds muscle, which acts as a metabolic sink for glucose.
Reclaiming Your Health Autonomy
High cholesterol is often a symptom, not a disease. [2]
Your body produces cholesterol in response to inflammation, stress, or injury. Treating the cholesterol without addressing the root cause is like turning off the smoke alarm instead of putting out the fire.
Do not stop medication without consulting your doctor. Statins have legitimate uses for people with established heart disease or very high risk. But if you’re taking statins for primary prevention (you’ve never had a heart attack), ask your doctor these questions.
- What’s my Absolute Risk reduction? Not Relative Risk. Absolute.
- What’s my NNT? How many people need treatment for one person to benefit?
- What’s my CAC score? Do I have actual plaque, or just elevated cholesterol?
- Have you checked my HbA1c, hs-CRP, and Triglyceride-to-HDL Ratio?
Demand the right tests. Focus on root causes. Insulin resistance, chronic inflammation, and oxidized LDL drive disease. Total cholesterol is a distraction.
Arm yourself with this data. Your doctor works for you, not pharmaceutical companies. If they dismiss your questions or refuse to order a CAC scan, find a doctor who listens.
Your life depends on asking the right questions.
Frequently Asked Questions
Citations
- [1] Ramsden CE, Zamora D, et al. – “Re-evaluation of the traditional diet-heart hypothesis: analysis of recovered data from Minnesota Coronary Experiment (1968-73)” – BMJ, April 2016 – DOI: 10.1136/bmj.i1246
- [2] Harvard Nutrition Source – “Research Review: Old data on dietary fats in context with current recommendations” – March 2025
- [3] Diabetes.co.uk – “Rediscovered study from 60s Minnesota shows up ‘heart healthy diet’ myth” – September 2022
- [4] Scientific American – “Records Found in Dusty Basement Undermine Decades of Dietary Advice” – February 2024
- [5] ResearchGate – “Re-evaluation of the traditional diet-heart hypothesis: Analysis of Recovered data from Minnesota Coronary Experiment (1968-73)” – April 2016
- [6] Chicago Tribune – “The heretical Minnesota heart study: When science stops asking questions” – May 2019
- [8] Montana Public Radio – “Forty Years In The Sugary Desert: Suppressed Science And The American Diet” – November 2021
- [10] Frantz ID Jr., et al. – “Test of Effect of Lipid Lowering by Diet on Cardiovascular Risk” – Arteriosclerosis, 1989
- [11] TheNNT – “Statins in Persons at Low Risk of Cardiovascular Disease” – March 2023
- [12] STAT News – “What are the odds that your medication will help you get better?” – June 2023
- [14] American Academy of Family Physicians – “Looking at the Benefit of Statins from a Different Perspective” – October 2010
- [15] American Heart Association – “Number Needed to Treat With Rosuvastatin to Prevent First Cardiovascular Events” – Circulation, 2009
- [24] UCLA Health/ScienceDaily – “Most Heart Attack Patients’ Cholesterol Levels Did Not Indicate Cardiac Risk” – November 2025
- [25] Harvard Health – “Heart attack despite low cholesterol?” – December 2015
- [26] UCLA Health – “Most heart attack patients’ cholesterol levels did not indicate cardiac risk” – January 2009
- [28] CardioSmart/American College of Cardiology – “Half of Patients with Ideal Cholesterol Have Underlying Heart Risks” – 2017
- [29] Johns Hopkins Medicine – “Study Suggests ‘Remnant Cholesterol’ As Stand-alone Risk for Heart Attack and Stroke” – September 2021
- [30] Sachdeva A, et al. – “Lipid levels in patients hospitalized with coronary artery disease” – American Heart Journal, January 2009
- [31] UCLA Health – “Ask the Doctors – Should I take CoQ10 with my statin?” – March 2018
- [32] Cleveland Clinic – “What To Know About CoQ10 and Statins” – January 2025
- [33] American Journal of Cardiology – “Effect of Coenzyme Q10 on Myopathic Symptoms in Patients Treated With Statins” – May 2007
- [35] NIH/PMC – “Coenzyme Q10 as Treatment for Statin-Associated Muscle Symptoms” – 2018
- [36] NIH/PMC – “Reversal of statin-induced memory dysfunction by co-enzyme Q10: a case report” – 2015
- [37] American Heart Association – “Effects of Coenzyme Q10 on Statin‐Induced Myopathy: An Updated Meta‐Analysis” – Journal of the American Heart Association, 2018
- [38] NIH/PMC – “Coenzyme Q10 and Statin-Induced Mitochondrial Dysfunction” – 2011
