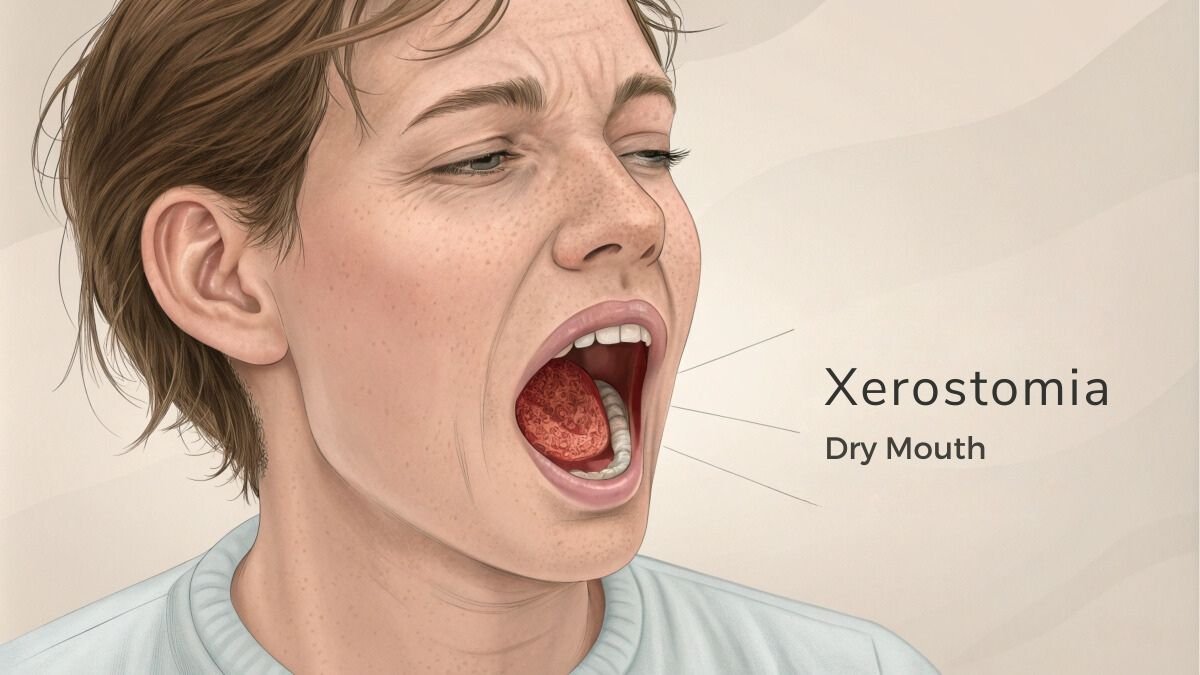
5 Ways Hyperbaric Oxygen Therapy Eases Xerostomia
Here are 5 research based ways Hyperbaric oxygen therapy combats xerostomia (dry mouth).
Hyperbaric oxygen therapy (HBOT) can effectively relieve your xerostomia symptoms through five key mechanisms.
- You’ll experience improved tissue regeneration as HBOT activates fibroblasts and increases stem cell production.
- The therapy boosts your saliva production by stimulating new blood vessel growth in damaged salivary glands, with benefits lasting up to 3.8 years.
- You’ll notice reduced inflammation thanks to high-pressure oxygen delivery and antioxidant effects.
- HBOT improves blood flow up to 400%, creating ideal healing conditions for your salivary glands.
- The treatment also helps prevent infections while protecting against dental complications.
In this article, I will explain in easy-to-understand language how these key mechanisms work according to scientific research. Understanding these mechanisms reveals how HBOT can transform your dry mouth treatment journey.
How Hyperbaric Oxygen Therapy Helps With Xerostomia (Dry Mouth)

1. Tissue Regeneration and Healing
Hyperbaric oxygen therapy (HBOT) is a great way to help with dry mouth, especially for people who have had radiation treatment for head and neck cancer.
During HBOT, you breathe pure oxygen in a special high-pressure room or chamber, which boosts your body’s natural healing. This therapy helps your body repair tissues by activating cells that produce collagen – essential for rebuilding damaged tissue.
It also moves stem cells from your bone marrow to where they’re needed, helping renew tissues. [1] [2]
Research shows that HBOT can significantly improve how well your salivary glands work. One study with patients who had radiation for head and neck tumors found that after 20 sessions of HBOT, the amount of saliva they produced nearly doubled, and the saliva’s acidity decreased, making it healthier. There was also a drop in harmful bacteria and fungi in the mouth, which can help prevent cavities. [3]
Another study looked at head and neck cancer patients who had 30 sessions of HBOT. These patients reported feeling much less dry mouth, and their saliva production increased slightly. For many, the improvement was enough to bring them out of the severely dry-mouth category. [4]
These studies suggest that HBOT not only makes dry mouth symptoms better but also helps repair the salivary glands themselves. This makes HBOT a beneficial treatment for anyone struggling with radiation-induced dry mouth.
2. Saliva Production Enhancement
Hyperbaric Oxygen Therapy (HBOT) can really help with dry mouth by boosting saliva production in a few different ways, making life a lot more comfortable for patients.
First off, HBOT helps heal and regenerate damaged salivary glands by delivering lots of oxygen to the affected areas. This extra oxygen helps grow new blood vessels in tissues that might have been damaged by radiation, which is super important for getting those tissues working properly again. [5]
Studies show that HBOT not only increases the amount of saliva you produce but also helps keep your saliva at a healthy pH, which is good for your overall mouth health. (The normal pH range for saliva is 6.2 to 7.6.). [5]
The treatment typically involves 30 sessions over six weeks, with each session lasting 90 minutes at a certain pressure level. Clinical studies have shown that patients see a noticeable increase in saliva, with one study noting an average increase of 0.9 mL over a 5-minute period. [6]
Plus, the good news is that the benefits of HBOT can last for years, with improvements seen up to 3.8 years after the therapy.
The reason HBOT works so well is that it helps create strong oxygen levels in injured tissues, which promotes natural healing. This is especially important for people who have severe dry mouth symptoms due to salivary gland damage from radiation therapy.
3. Inflammation Reduction
Hyperbaric Oxygen Therapy (HBOT) can really help manage dry mouth by reducing inflammation and boosting the body’s healing processes, which in turn improves saliva production.
Inflammation is a common cause of reduced saliva production, often seen in conditions like Sjögren’s syndrome and other issues with salivary glands. [7]
When there’s inflammation, the salivary glands don’t work as well, leading to dry mouth. [8]
HBOT helps by lowering levels of substances that cause inflammation, like certain proteins in the body. [9]
By decreasing these inflammatory proteins, HBOT reduces the inflammation that interferes with the salivary glands’ ability to produce saliva.
Additionally, HBOT also addresses oxidative stress, which is another big factor in inflammation. Oxidative stress happens when the body produces too many free radicals, which can damage cells and tissues, leading to more inflammation. HBOT helps reduce these harmful free radicals, making it easier to control inflammation. [10] [11]
It also boosts the release of substances that aid in tissue repair and the formation of new blood vessels. These substances not only help heal damaged tissues but also reduce inflammation further.
With increased oxygen levels in tissues thanks to HBOT, cells can repair and function better, which helps restore normal salivary gland function and boosts saliva production.
Studies have shown that other treatments like special anti-inflammatory substances and artificial saliva can also help by reducing inflammation and promoting saliva secretion. [12]
So, by lowering inflammation, reducing oxidative stress, and enhancing tissue repair, HBOT provides a well-rounded approach to managing dry mouth and improving oral health.
4. Blood Flow Improvement

Hyperbaric Oxygen Therapy (HBOT) increases oxygen levels in your tissues and blood vessels significantly. This extra oxygen helps improve blood flow, especially in tissues that may have been damaged by radiation therapy. With better blood flow, more oxygen and nutrients can reach your tissues, aiding in their repair and function.
Another way HBOT helps is by promoting the formation of new blood vessels. It boosts the production of cells and substances needed to create these vessels, enhancing blood supply to areas that might be suffering from limited blood flow, like those affected by certain conditions. [13]
Now, let’s talk about how this improved blood flow helps alleviate xerostomia, or dry mouth.
Better blood circulation means that the salivary glands receive more oxygen and nutrients, helping them function more effectively. This can lead to increased production of saliva, which helps with the symptoms of dry mouth.
Not only do the salivary glands work better, but the quality and quantity of saliva production can also improve. This provides much-needed relief from the discomfort and complications associated with dry mouth.
So, by improving blood circulation and reducing inflammation, HBOT supports the health and functionality of the salivary glands, offering a promising treatment for those suffering from dry mouth.
5. Infection Prevention and Control
Dry mouth, or xerostomia, can be caused by infections and various diseases. Chronic hepatitis C can lead to dry mouth due to issues with the salivary glands. Bacterial infections can also cause dry mouth by affecting immune cells. While herpesviruses might not directly cause dry mouth during radiotherapy, other viral infections can still lead to oral dryness.
Autoimmune diseases like Sjögren’s syndrome often affect salivary glands, causing dry mouth. Diabetes can lead to dry mouth due to dehydration and metabolism changes. Renal failure can cause dry mouth from dehydration and protein buildup. Graft-Versus-Host disease can damage salivary glands, leading to dry mouth.
Studies have shown that hyperbaric oxygen therapy (HBOT) can be effective in treating infections by enhancing the body’s ability to fight off bacteria and other pathogens. [14]
Since HBOT boosts the immune system and works well with certain antibiotics, it’s particularly useful for deep and chronic infections. So, by reducing inflammation and limiting tissue damage, HBOT can also prevent infections from spreading like the ones that cause Xerosotomia.
Understanding and Managing Xerostomia (Dry Mouth)
Xerostomia, commonly known as dry mouth, happens when your mouth doesn’t produce enough saliva. This can affect both your oral health and overall well-being. Common causes include medications, radiation therapy, systemic diseases, and autoimmune conditions like Sjögren’s syndrome.
Causes of Xerostomia
- Medications: Many widely prescribed drugs can cause dry mouth as a side effect. This includes medications with anticholinergic properties, which block certain nerve signals.
- Radiation Therapy: Treatments for head and neck cancers can damage salivary glands, reducing saliva production.
- Systemic and Autoimmune Diseases: Conditions like Sjögren’s syndrome, diabetes, and rheumatoid arthritis are linked to dry mouth. These diseases often cause inflammation or damage to the salivary glands.
- Hormonal Changes: Changes in hormone levels, particularly in menopausal women, can also lead to dry mouth.
How Xerostomia Develops
- Salivary Gland Dysfunction: Saliva production is controlled by your nervous system. When these nerves are damaged or malfunction, it can lead to dry mouth.
- Cellular and Molecular Pathways: The process of saliva production involves complex interactions between cells and neurotransmitters. Disruptions in these pathways can prevent saliva from being made, resulting in dry mouth.
Impact and Management
- Oral Health Complications: Dry mouth can lead to problems like tooth decay, oral infections, and difficulties with dentures, all of which can seriously affect your quality of life.
- Management Strategies: Treatment usually focuses on relieving symptoms and addressing the root causes. This can include using saliva substitutes, medications to stimulate saliva production, and maintaining good oral hygiene with regular dental visits and fluoride use.
Conclusion
Xerostomia is a condition with many causes, including medications, radiation therapy, and systemic diseases. Understanding why it happens and how it develops is important for effectively managing it and improving patients’ lives.
You’ll find hyperbaric oxygen therapy offers real hope for managing xerostomia symptoms. By boosting tissue healing, enhancing saliva production, and reducing inflammation, HBOT can greatly improve your quality of life. The therapy’s ability to increase blood flow and fight infections makes it a valuable treatment option. Consider discussing HBOT with your healthcare provider to determine if it’s right for your dry mouth concerns.
More Research Based articles on HBOT
